Crohn’s vs Celiac Disease: Key Differences and Similarities
Danielle Gaffen, MS, RDN, LD
- Last Updated
Both celiac disease and Crohn’s disease are chronic inflammatory conditions of the gastrointestinal tract. Learn key things to know about Crohn’s vs. celiac disease.
While symptoms can be similar, these two autoimmune diseases have different causes, triggers, treatment, and nutritional recommendations. This blog provides key differences and similarities between the conditions.
Crohn’s disease vs celiac disease
Let’s dive into how these two diseases can impact your health, and how your food choices play a role.
What is Crohn’s disease?
More than half a million people in the United States are estimated to have Crohn’s disease. Crohn’s disease is a type of inflammatory bowel disease (commonly abbreviated as IBD). To avoid additional confusion between Crohn’s vs. celiac vs. IBS, learn more about IBD vs. IBS).
Crohn’s disease can affect any part of the GI tract from the mouth to the anus, but most commonly affects the end of the small intestine (ileum) and the beginning of the colon. And inflammation of the intestine can “skip,” or leave normal areas in between patches of diseased intestine. It can affect the entire thickness of the bowel wall.
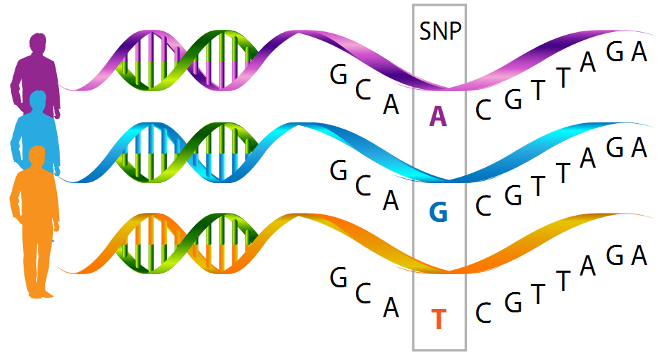
No one factor has been identified as causing Crohn’s disease. Rather, researchers have identified at least four factors that may contribute to developing the condition:
- Genetics
- the gut microbiome
- the immune system
- an environmental trigger
Food triggers are a concern for many people with Crohn’s disease, as certain foods may be more likely to cause inflammation, flare-ups, and symptoms for some people. While there are some food triggers that are more common for people with Crohn’s disease, different foods appear to affect different guts differently with this condition.
What is Celiac Disease?
2 million people in the United States are estimated to have celiac disease. Celiac disease is an autoimmune disease. Eating foods containing gluten, the protein in wheat, rye, and barley, causes a person’s own immune system to attack and damage the small intestine.
These attacks can cause symptoms like cramping and diarrhea, but damage to the small intestine can also disrupt a person’s ability to absorb nutrients from food.
Similar Symptoms of Crohn’s vs Celiac Disease
Overlapping symptoms between Crohn’s disease and celiac disease include:
- abdominal pain
- anemia
- diarrhea
- fatigue
- fever
- joint or muscle pain
- nausea or vomiting
- rectal bleeding
- short stature
- weight loss
These similar symptoms mean that it can be difficult to tell the conditions apart without diagnostic testing. To confirm a diagnosis of either, a doctor will likely order blood tests, a biopsy, endoscopy, and other tests.
Is it Possible to Have Both Celiac and Crohn’s Disease?
Even with some conflicting data, most studies conclude that celiac disease is more common in IBD patients. Researchers believe the prevalence of Crohn’s disease is higher than ulcerative colitis in patients with celiac disease.
Conversely, a meta-analysis published in 2020 in the journal Gastroenterology, which involved more than 60 individual studies, showed that people with celiac disease are almost 10 times as likely to have IBD, including Crohn’s disease and UC — compared with people who don’t have celiac disease.
With this increased prevalence and many similar symptoms, some researchers suggest that patients over the age of 40 who are anemic or have chronic diarrhea, and are diagnosed with celiac disease, should also have a colonoscopy to test for IBD.
Still, even though Crohn’s and celiac disease may be related, having one condition doesn’t mean you’ll develop the other.
Can Celiac Disease be Mistaken for Crohn’s Disease?
Because similar symptoms like abdominal pain and diarrhea may be present in both diseases, telling the difference between Crohn’s disease and celiac disease can be difficult. Medical doctors often use blood tests, endoscopies and/or biopsies to determine which disease is present.
Please note: it’s important to not start a gluten-free diet before completing these tests, otherwise some of the labs tested may come back normal and you won’t receive a proper diagnosis.
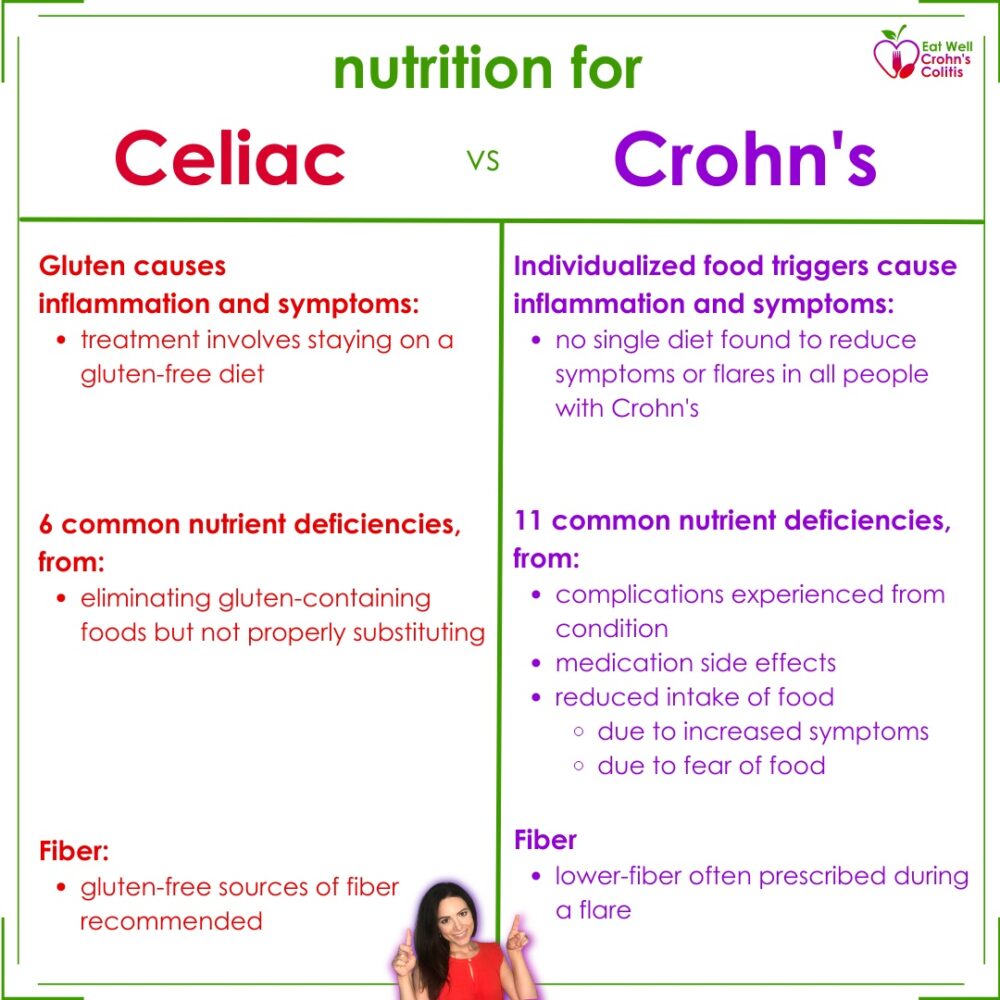
Here’s a chart comparing nutrition for celiac disease versus Crohn’s disease:
Celiac Disease Diet
If the diagnosis is celiac disease, treatment involves staying on a gluten-free diet.
Gluten-free nutrition therapy will allow the intestine to heal. It also will help prevent complications like bone disease that can happen if celiac disease goes untreated.
A person with celiac disease should carefully read all food labels and ingredient lists to see if the food contains wheat, barley, or rye. Although many sources of these grains will be obvious to you, others may not.
Crohn’s Disease Diet
Unlike with celiac disease, eating gluten does not cause inflammation in all people with Crohn’s disease. However, depending on the individual, certain foods can worsen symptoms.
According to a study published in the journal Inflammatory Bowel Disease, almost 20% of IBD patients have tried a gluten-free diet, and 65% of those found a subjective benefit for their GI symptoms.
If you have Crohn’s disease, you might not be able to digest all the food you eat, so you may need more vitamins and minerals. Your medications might also affect your ability to eat or how your body absorbs nutrients.
How much fiber you should eat depends on your symptoms and the amount of inflammation in your intestines. If you are taking prednisone or budesonide medications, then you should limit the amount of fiber that you are eating. If you are experiencing symptoms like diarrhea, abdominal pain, low-fiber foods are the easiest to digest and are less irritating for your intestines.
If you don’t have symptoms, then check with your health care provider or registered dietitian nutritionist (RDN) to see if you may add more fiber to your diet. It’s also important to eat enough protein foods while you are on the IBD diet.
Diet Tips for Celiac Disease
If you have celiac disease, keep these nutritional recommendations in mind:
- Make sure you get enough of certain nutrients. Specifically B-vitamins (thiamin, riboflavin, niacin, and folate), iron, and fiber.
- Choose whole grain, gluten-free products whenever possible. Look for products containing whole grain corn, whole grain rice, millet, teff, or sorghum.
- Choose enriched, gluten-free products instead of refined, unenriched products whenever possible. There are many companies that produce enriched, gluten-free products.
- Eat more foods made with alternative plant foods, such as amaranth, quinoa, and buckwheat. These plant foods are good sources of fiber and iron as well as some B-vitamins.
- Eat other enriched, gluten-free foods such as enriched rice.
- Make sure to eat plenty of non-grain sources of the nutrients your body needs. For example:
- Lean cuts of fresh pork, legumes (dry beans, peas, lentils), nuts, and fish are good sources of thiamin.
- Dairy products, legumes, nuts, green leafy vegetables, and mushrooms are good for riboflavin.
- Eat poultry, fish, lean cuts of fresh pork, legumes, and seeds for niacin.
- Choose legumes, green leafy vegetables, and fruit juices for folate.
- You can get iron from lean cuts of beef, poultry, seafood, legumes, dried fruits, green leafy vegetables, nuts, and seeds.
- All plant foods—fruits, vegetables, legumes, seeds, and nuts—are good sources of fiber.
- Consider taking a gluten-free multivitamin and mineral supplement.
Diet Tips with Crohn’s disease
Because no one diet has been shown to work for everyone with Crohn’s disease, here are some general Crohn’s diet tips to consider:
- Eat small meals or snacks every 3 or 4 hours. Do not skip meals.
- Be aware of fiber. When you have symptoms, or if you are taking prednisone or budesonide, foods that are lower in fiber may be better tolerated.
- Consider whole grains, fruits, and vegetables when appropriate. When you don’t have symptoms (no blood in your stools), you are no longer taking prednisone or budesonide, and your inflammation is mild, your health care provider may recommend that you begin including whole grains and a variety of fruits and vegetables in your diet.
- Eat a protein food or dairy product at every meal or snack if your body can tolerate it.
- Drink a lot of fluids, at least 8 cups each day. Limit caffeinated, sugary drinks, and beverages made with sugar substitutes.
- Eat foods that have probiotics (like yogurt and kefir) and prebiotics (like bananas). Check with your health care provider before starting probiotic or prebiotic supplements.
- Take a multivitamin with minerals, if needed. Ask your RDN for recommendations.
- If you are taking methotrexate or sulfasalazine, take one multivitamin with minerals and a supplement with 1 milligram of folic acid daily.
- Consider a calcium + vitamin D supplement. Take a calcium supplement with vitamin D if you are not getting enough calcium from your diet.
Take Home Messages: Crohn’s vs. Celiac
- Crohn’s disease and celiac disease are two chronic inflammatory conditions. The difference in symptoms is often not significant enough to tell the difference between the two diseases.
- While similar in symptoms, they have different causes, triggers, diagnostic criteria, and nutritional recommendations.
- Speak with your healthcare team if you experience symptoms of Crohn’s or celiac for a formal diagnosis so that you can receive appropriate treatment and nutritional recommendations.
All included information is not intended to treat or diagnose. For medical questions, please consult your healthcare provider.
Looking to learn more about nutrition for IBD? Check out this blog, “Is Alcohol Good for Crohn’s Disease and Ulcerative Colitis?”