IBD vs IBS: What’s the Difference?
Danielle Gaffen, MS, RDN, LD
- Last Updated
Co-written by Ranjani Priya Ravinuthala, MS, RDN
While IBD and IBS are similar sounding acronyms, this blog explores the key differences between the two gut conditions: IBD vs IBS.
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two distinct gastrointestinal disorders, though the differences between the two can be confusing for many people. Although some of the symptoms may be similar, these two health conditions are VERY different. This guide will compare both conditions, as well as demonstrate how nutritional recommendations are different for each condition.
IBD vs. IBS: Key Differences
Inflammatory bowel disease (IBD) is an umbrella term used to describe conditions that involve chronic inflammation of the digestive tract. In inflammatory bowel disease, the inflammatory response results in gastrointestinal tissue damage. The clinical course of the disease may be mild and episodic, or severe and unremitting. The two major forms of inflammatory bowel disease are Crohn’s disease and ulcerative colitis, or UC.
Irritable bowel syndrome (IBS) is a functional GI disorder. This means that the condition is caused by changes in the way the GI tract works, as opposed to a physical abnormality in the GI tract (like in Crohn’s disease or UC).
What is Inflammatory Bowel Disease?
An estimated 1.3% (or 3 million) of US adults reported being diagnosed with IBD. Men and women are equally likely to be affected by the disease.
While IBD can affect each person a little differently, these are some of the more common symptoms:
- Persistent diarrhea
- Rectal bleeding
- Urgent need to move bowels
- Abdominal cramps and pain
- Constipation
- Nausea
- Vomiting
While IBD involves inflammation in the GI tract, it can affect your overall health and cause more serious medical issues. For example, loss of appetite, weight loss, low energy and fatigue, nutrient deficiencies, fissures, fistulas, strictures, blockages, and osteoporosis. And these medical issues can impact nutritional recommendations!
How are Crohn’s Disease and Ulcerative Colitis Different?
Crohn’s disease may involve any part of the GI tract from mouth to anus, but approximately 50-60% of cases involve the distal ileum and the colon. In Crohn’s disease, segments of inflamed bowel may be separated by healthy segments.
In ulcerative colitis, disease activity is limited to the large intestine and rectum and the disease process is continuous.
What is IBS?
An estimated 10-20% of the United States population has IBS, with about twice as many women as men being affected.
IBS is characterized by unexplained abdominal discomfort or pain that is associated with changes in bowel habits.
Other common symptoms include:
- gas
- bloating
- diarrhea and constipation
- increased GI distress associated with psychological and social stress
IBS Subtypes
IBS subtypes are based on the predominant bowel habits and stool form.
IBS-D
Irritable Bowel Syndrome with increased symptoms of watery stools and diarrhea is known as IBS-D.
IBS-C
Irritable Bowel syndrome with constipation is another common form of IBS which is associated with passing hard stools. People experience gas, bloating, straining, painful bowel movements and abdominal pain.
IBS-M
IBS-M is mixed IBS is irritable bowel syndrome mixed which is going back and forth with diarrhea and constipation.
IBS-U
IBS-U, or Unclassified IBS is defined as a patient who meets diagnostic criteria for IBS but whose bowel habits cannot be accurately categorized into the other 3 subgroups. This is when the patient reports that they rarely have abnormal stools.
Diagnosing IBD and IBS
For IBD, a combination of the following procedures could be used to diagnose the condition:
- Endoscopies: like a colonoscopy, flexibly sigmoidoscopy, upper endoscopy, capsule endoscopy, or balloon-assisted enteroscopy.
- Imaging scans: like an X-ray, CT scan, or MRI.
- Lab tests: like stool cultures or blood tests to check for inflammation or markers that could be abnormal.
There are currently no pathophysiological tests available to adequately diagnose IBS. Instead, after the exclusion of other gastrointestinal diseases (such as IBD), symptoms play an important role in establishing a positive diagnosis. IBS should be diagnosed by a medical doctor, who should take a careful history and use the Rome IV criteria. These allow IBS to be classified by the predominant symptom type, into: IBS-C, IBS-D, IBS-M, and IBS-U.
Flare-Ups with IBD and IBS
Many people with IBD and IBS will experience a flare-up of symptoms that often leads to a diagnosis, although intermittent flare-ups continue after diagnosis as well. Flare-ups are usually when many symptoms become more apparent after a period of remission, such as pain and needing to use the restroom more often.
Nutrition Strategies for IBD
Nutrition for IBD
People with IBD are at increased risk of nutrition problems for a host of reasons related to the disease and its treatment. And medical nutrition therapy can look very different for a person depending on their specific situation.
For example, if someone with Crohn’s has severe strictures, the nutritional recommendations are going to look different than someone with UC who just had a colectomy and now has an ostomy.
Diets for IBD
As of right now, there is no single diet or eating pattern for reducing symptoms or decreasing the flares in all people with IBD.
While different elimination diets are being researched for IBD, currently no one diet has been shown to help all people with IBD.
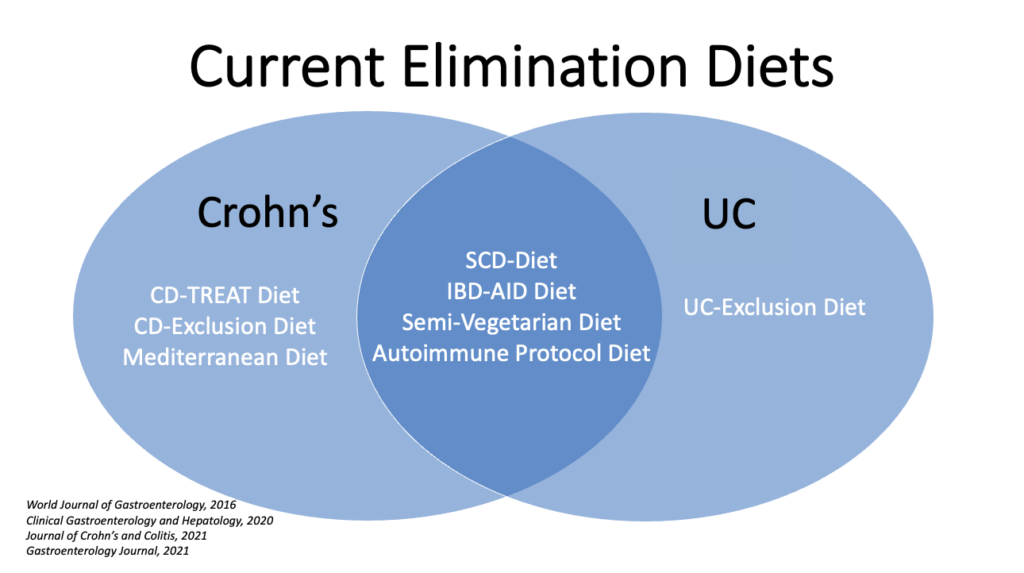
Here’s a Venn Diagram I made with the variety of eating patterns from nutritional research publications that are starting to be studied in greater detail. These elimination diets may work for some people, as research methods are improving, and some are showing some promising results. But these eating patterns can also be very restrictive, and none of these diets have been proven to work for everyone with IBD.
What we know right now is that many people with IBD report specific, individualized food triggers or intolerances. But different guts tolerate different foods differently with this condition!
A good example of this is my husband with Crohn’s…he is completely lactose intolerant…we learned that even the tiniest amount of lactose is going to cause him a bad time. But I have worked with many clients who tolerate dairy fine, and one client even tolerated dairy products BEST! So at this time, it appears that different guts tolerate different foods differently!
Nutrition Strategies for IBS
Nutrition for IBS
Just as there is no single therapy for treating IBS, it’s important to remember there’s no single dietary strategy either. However, a growing amount of research suggestions that the low-FODMAP diet is an eating pattern that has improved symptoms and quality of life for many people with IBS.
What is the Low FODMAP Diet?
The low-FODMAP elimination diet used to identify people with IBS’ problem foods. It’s a short term diet, based on limiting certain short-chain carbohydrate-containing foods, including sugars, starches, and fibers that some people can’t fully digest and absorb. These short-chain carbohydrates are poorly absorbed in the small intestine, resulting in gas, pain, and diarrhea in sensitive individuals. This diet has been shown to help most people with IBS.
Malnutrition and IBD
We can’t talk about IBD without talking about the HUGE risk for malnutrition. We care so much about malnutrition for IBD because it leads to poorer disease outcomes. Even mild cases of malnutrition can make it more difficult for the body to bounce back after an illness. Malnutrition compromises digestion and absorption function in the GI tract and can cause growth delays in children with IBD.
Some of the reasons why malnutrition is so prevalent in people with IBD are:
- complications experienced from the condition: abscesses, fistulas, strictures, ostomies, and beyond. This blog won’t be diving deep into the nutrition recommendations for each of these complications, but it can be very confusing for a patient to know what to eat if they develop a complication like this.
- medication side effects: IBD warriors may be taking quite an extensive list of prescription medications, many of which have big nutritional side effects.
- reduced intake of food: either during a flare from increased symptoms or from a fear of food brought on by a fear of negative consequences after eating said food.
All these reasons can lead to an overly restricted diet and increases the likelihood of malnutrition and weight loss.
Nutrient Deficiencies Commonly Found in IBD
60-75% of people with IBD will experience one or more deficiencies.
Several nutrient deficiencies are common for both Crohn’s disease and UC, like iron, folate, magnesium, calcium, and potassium. However, in Crohn’s disease, because the inflammation and disease process affect the small intestine and not just the colon, additional nutrient deficiencies like vitamin B12, vitamins A, D, E, and K, and zinc are commonly deficient.
I can share that iron, vitamin D, and B12 are the big three deficiencies I see repeatedly in my private practice.
Nutritional Deficiencies Common in IBS
It is important to be aware that common nutritional deficiencies can arise with the low FODMAP diet if foods that are eliminated are not substituted with comparable items. Common nutritional deficiencies include:
- folate, thiamin, and vitamin B6 (from limiting cereals and breads)
- calcium and vitamin D (from avoidance of dairy products)
Medical Management of IBD vs IBS
Medical Management of IBD
The goals of treatment in IBD are to induce and maintain remission and to improve nutrition status.
Currently, the most effective medical agents include corticosteroids, anti-inflammatory agents, immunosuppressive agents, antibiotics, and anti-TNF agents.
Surgical Management of IBD
In Crohn’s disease, surgery may be necessary to repair strictures or remove portions of the bowel when medical management fails. Approximately 50-70% of persons with Crohn’s disease undergo surgery related to the disease. Surgery does not cure Crohn’s disease, and recurrence often occurs within 1 to 3 years of surgery. The chance of needing subsequent surgery in the patient’s life is approximately 30-70%, depending on the type of surgery and the age of the first operation.
This is important from a nutritional perspective because major resections of the intestine may result in varying degrees of malabsorption of fluid and nutrients.
For example, in most Crohn’s cases, the disease activity occurs in the ileum. So, if a patient needs the majority her ileum removed, she may need to get her vitamin B12 lab values checked regularly.
With UC, approximately 20% of patients have a colectomy (removal of the colon), and this resolves the disease because without the colon, there is no more colon to be chronically inflamed. Whether a colectomy is necessary depends on the severity of the disease and indicators of increased cancer risk. After a colectomy for UC, surgeons may create an ileostomy with an external collection pouch or an internal abdominal reservoir fashioned with a segment of ileum or an ileoanal pouch, which spares the rectum, to serve as a reservoir for stool.
Medical Management of IBS
There is no specific therapy that works for all people with IBS. Generally, the treatment option is determined by the predominant bowel pattern and the symptoms that most disrupt the patient’s quality of life. For example, different medications, dietary interventions, and/or mind-body therapies would be recommended if a person has IBS-D compared with IBS-C. Many people find that with these changes, symptoms improve and can be managed for long periods of time.
Take Home Message about IBD vs. IBS
Despite having similar acronyms and symptoms, the similarities between IBS and IBD stop there. Because of this, it is essential to get an accurate diagnosis, as treatments and nutritional recommendations for these conditions are very different. Make an appointment with your healthcare team if you think you might have either (or both) of these conditions.
This article was originally published on December 3, 2021 and has been updated with new diet research.











































