Is Ulcerative Colitis a Disability?
Danielle Gaffen, MS, RDN, LD
- Last Updated
Co-written by Renata Cauchon-Robles
If you or someone you know is living with ulcerative colitis, you know the challenges of certain daily activities. A common question we get is, is ulcerative colitis a disability? This blog will help you better understand the answer to this question, with helpful tips to help you thrive.
Symptoms of ulcerative colitis often aren’t predictable. Managing symptoms at work or school can be extra tricky. Luckily, there are adjustments and accommodations available that can help manage symptoms and support a good quality of life.
In various settings such as schools, airports, and workplaces, individuals with ulcerative colitis can seek specific accommodations that can help with symptom management. This blog will explain a few examples, including specifics for work and school environments to traveling, that you may find extra useful to know about.
The ABC of Healing and Establishing a Robust Treatment Plan
Managing ulcerative colitis starts with a comprehensive treatment plan tailored to your unique needs. A recent study pointed out that the need for disability accommodations decreased when IBD patients had more advanced healing in their intestinal lining. This plan is key to lessening the impact of UC on daily activities and may reduce the need for certain accommodations. Here are a few considerations:
A) Personalized Medication Strategy
Partner with your gastroenterologist to find the right balance of medications. This may include anti-inflammatory drugs, immune system suppressors, or biologics tailored to your specific condition.
B) Tailored Diet and Nutrition
Work with a registered dietitian nutritionist that specializes in IBD to craft a diet that helps minimize your symptoms while ensuring a balanced diet. Remember, the goal is to identify your unique dietary triggers and create a plan that fits practically into your lifestyle.
C) Ongoing Medical Supervision
Engage in regular check-ups with your healthcare team to track the progress of your healing and make necessary adjustments to your treatment protocol.
Can You Get Disability for Ulcerative Colitis?
While there isn’t a specific Ulcerative Colitis Disability Act, section 5.00 of the Social Security Disability Evaluation Under Social Security includes Digestive Disorders, such as ulcerative colitis.
Since symptoms can vary week to week, and having severe ulcerative colitis isn’t necessarily permanent, it can be hard to categorize as a disability.
In many places, there are legal protections in place to ensure that individuals with chronic conditions like ulcerative colitis can request reasonable accommodations under disability laws.
For example, in the United States, the Americans with Disabilities Act (ADA) and Section 504 of the Rehabilitation Act can provide a legal basis for such accommodations in schools, workplaces, and other settings. This underscores the importance of understanding and addressing the question, is ulcerative colitis a disability? These laws reflect a commitment to ensuring that people with UC have access to the accommodations they need to participate fully in all aspects of life.
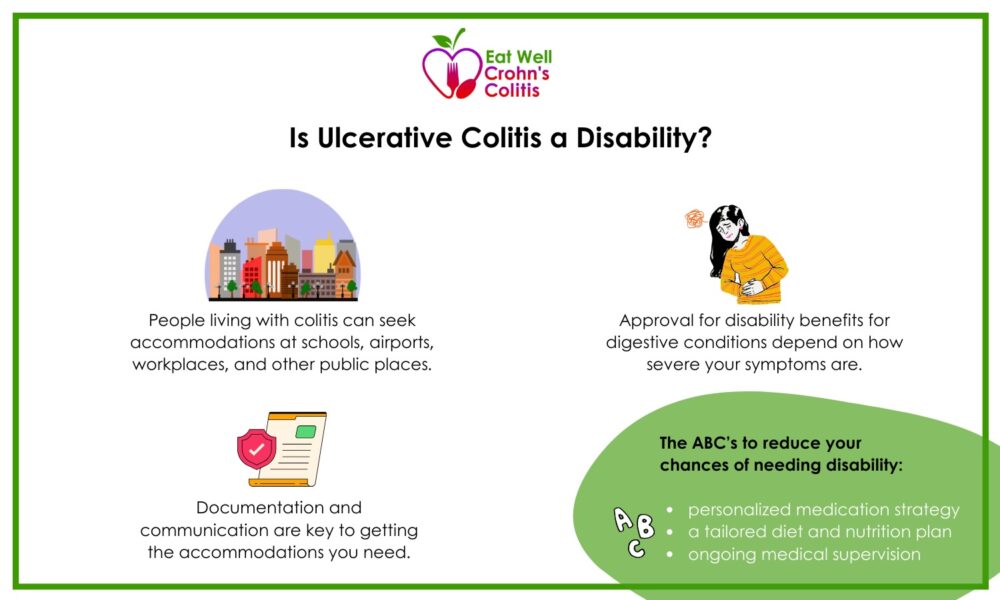
Chances to Win Social Security Disability with Ulcerative Colitis
Qualifying for disability for ulcerative colitis may depend on how severe your symptoms are. You can qualify for Social Security disability payments with ulcerative colitis, if it has interfered with your ability to work. The amount you receive will depend on the severity, and your personal work history.
Keep in mind that the Social Security Administration requires documentation to show the ways ulcerative colitis is preventing you from working on an ongoing basis. You can apply for both Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) to see if you qualify.
Veterans with Ulcerative Colitis: VA Rating
Getting a VA rating can help Veterans with ulcerative colitis get adequate benefits. Your ulcerative colitis status will determine where your VA rating falls (10%, 30%, 60%, or 100%). For example, if someone is experiencing malnutrition with multiple flares a year, a 60% VA Rating may be available.
Can You Work with Ulcerative Colitis?
Many people hesitate going to work with ulcerative colitis symptoms, but it’s definitely still possible.
Navigating dietary and nutritional needs in various settings often requires open communication and sometimes advocacy. Individuals may need to provide medical documentation or letters from healthcare providers to formalize accommodation requests.
Patient advocacy organizations, like the Crohn’s & Colitis Foundation, can offer guidance and support in securing accommodations, too.
A Smooth Workday with Ulcerative Colitis
If you’re wondering how to get through the workday when you’re managing ulcerative colitis symptoms, the first step is finding out what you need to get through the day comfortably.
Consider your commuting options, bathroom access, your paid leave options, and social support. Your schedule and cold storage for medication are also important to consider.
Flexible Work Schedule
Having flexibility around meals can make a big difference, too. As an employee you can negotiate for flexible mealtimes or breaks to be able to eat snacks that align with your diet management plans.
Food and Medication Storage
In addition, the ability to store and refrigerate your food and medication in the workplace can be crucial for managing diet and symptom control. This might mean advocating for the refrigeration and storage options you need.
What Accommodations are Available in Schools?
Students of all ages who are managing ulcerative colitis symptoms can be supported by special accommodations in public or private schools. This may include flexibility around mealtimes, exams, or housing accommodations. Students may be allowed to eat snacks or meals at non-standard times to accommodate their dietary needs or to manage symptoms.
Colleges typically offer Disability Support Services that can support you in setting up accommodations for meals, class time, or housing arrangements.
In addition to the standard menu, K-12 schools are expected to provide meals that meet the nutritional needs of students with specific health conditions or dietary restrictions, such as ulcerative colitis.
Laws and Policies for Student Dietary Accommodations
The following laws recognize that conditions like ulcerative colitis can significantly impact a student’s diet and, therefore, require accommodations to ensure their nutritional needs are met.
National School Lunch Program (NSLP)
NSLP is a federally assisted meal program operating in public and nonprofit private schools. Participating schools are required to comply with federal regulations that include accommodating students with disabilities that restrict their diet or bowel functions. This includes episodic conditions that impact regular life activities.
This may include flexibility around mealtimes. Students may be allowed to eat snacks or meals at non-standard times to accommodate their dietary needs or to manage symptoms.
Americans with Disabilities Act (ADA), Section 504 of the Rehabilitation Act
The ADA and Section 504 are policies that require schools to provide reasonable accommodations for students with disabilities, including digestive concerns. Modifications to the standard meal program should be provided when requests are supported by medical documentation.
Traveling with Ulcerative Colitis
As someone with ulcerative colitis, you have permission to carry medications when you travel. You are allowed to carry medications including liquid medicines and nutritional supplements through airport security checkpoints. You just might need to declare them, or need to step through some additional screening.
If you have specific questions about foods and liquids needed during your flight, or how to handle your medications and nutritional supplements while traveling, the AskTSA team is available for support.
Is Ulcerative Colitis a Disability?
Anyone living with ulcerative colitis has the right to attend work and school, travel, and enjoy life’s pleasures just like anyone else. There are legal protections that support people with chronic conditions to receive accommodations at work and school. Advocating for what you need to get through the day comfortably is the first step to making it work.
Learn More
- Learn about how diet can help treat Ulcerative Colitis
- Track how your food links up with your Ulcerative Colitis symptoms
References
- Bram Verstockt, Lieven Pouillon, Florence Ballaux, Celine Jorissen, Eveline Hoefkens, Nikki Lembrechts, Peter Bossuyt, Patient-reported Outcomes and Disability Are Associated with Histological Disease Activity in Patients with Ulcerative Colitis: Results from the APOLLO Study, Journal of Crohn’s and Colitis, Volume 17, Issue 7, July 2023, Pages 1046–1054, https://doi.org/10.1093/ecco-jcc/jjad015
- Cheng L, Jetha A, Cordeaux E, Lee K, Gignac MAM. Workplace challenges, supports, and accommodations for people with inflammatory bowel disease: A scoping review. Disability and Rehabilitation: An International, Multidisciplinary Journal. 2022;44(24):7587-7599. doi:10.1080/09638288.2021.1979662
- 5.00-Digestive-Adult. www.ssa.gov. https://www.ssa.gov/disability/professionals/bluebook/5.00-Digestive-Adult.htm
- Sellin JH. Deconstructing Disability in Inflammatory Bowel Disease. Clinical Gastroenterology and Hepatology. 2014;12(8):1338-1341. doi:https://doi.org/10.1016/j.cgh.2014.02.033
- Is Ulcerative Colitis Considered a Disability? www.healthcentral.com. Published October 23, 2023. Accessed February 25, 2024. https://www.healthcentral.com/condition/ulcerative-colitis/is-ulcerative-colitis-a-disability
- You Can Get Disability for Ulcerative Colitis. Here’s How. | Atticus. www.atticus.com. Accessed February 25, 2024. https://www.atticus.com/advice/general/ulcerative-colitis-qualifies-for-disability-benefits-heres-how
- Veterans with IBD. Crohn’s & Colitis Foundation. Accessed February 25, 2024. https://www.crohnscolitisfoundation.org/patientsandcaregivers/community-support/veterans
- The Top 5 Ulcerative Colitis VA Rating Tips Explained (Ultimate Guide). Published October 14, 2022. Accessed February 25, 2024. https://vaclaimsinsider.com/ulcerative-colitis-va-rating/
- Can you pack your meds in a pill case and more questions answered | Transportation Security Administration. Tsa.gov. Published 2021. https://www.tsa.gov/travel/travel-tips/can-you-pack-your-meds-pill-case-and-more-questions-answered
- Accommodating Disabilities in the School Meal Programs: Guidance and Q&As | Food and Nutrition Service. www.fns.usda.gov. https://www.fns.usda.gov/cn/accommodating-disabilities-school-meal-programs-guidance-qas
- U.S. Department of Justice Civil Rights Division. Introduction to the Americans with Disabilities Act. ADA.gov. Published November 18, 2022. https://www.ada.gov/topics/intro-to-ada/
- U.S. Department of Education. Protecting students with disabilities. Edgov. Published online July 18, 2023. doi:http://www.ed.gov/about/offices/list/ocr/504faq.html











































