Food Additives: Which to Watch Out for with IBD
Danielle Gaffen, MS, RDN, LD
- Last Updated
Let’s be real, unless you’re cooking all of your food from scratch and consuming whole foods exclusively, you’re going to find yourself in the grocery aisle with a lot of products to choose from. So how do you ultimately choose which of the hundreds of products to buy?
Researchers are exploring whether food additives such as gums and emulsifiers may pose particular risks with respect to promoting inflammation and triggering disease activity in people with inflammatory bowel disease. Please find a list of some of the more questionable food additives below, based on the nutritional research, my professional experience, and my husband’s nutritional journey:
Fructose
New research suggests that eating a diet high in fructose can damage the colon and cause inflammation [1]. This finding suggests that a higher fructose intake may have played a role in the increased incidence of IBD in recent decades.
Fructose is the sweetest of all sugars, and the consumption of fructose has increased almost by one-third in the US over the past 3 decades, according to some estimates. The biggest source of fructose in the American diet is high fructose corn syrup, used because it’s very cheap. If you’re wondering what the heck high fructose corn syrup is, it’s a sweetener derived from corn syrup, which is processed from corn. It became a popular sweetener in the late 1970s when the price of regular sugar was high, while corn prices were low due to government subsidies.
Some examples of packaged foods that contain high fructose corn syrup are:
- soda
- candy
- sweetened yogurt
- salad dressings
- sauces
- condiments
- breads
- some canned fruits and juices
- granola bars and cereals
- snack foods
- nutrition bars
- coffee creamer
- energy or sports drinks
- jams or jellies
Take home message here is that all sorts of foods contain high fructose corn syrup in America, so reading the nutrition facts label may be helpful.
Gums
When I say gums here, I’m not referring to chewing gum, but the food gums you’ll see as ingredients in many packaged foods.
Many food gums and emulsifiers are naturally derived, like:
- Locust bean gum comes from the carob tree
- Guar gum is extracted from a type of legume known as cluster bean.
- Xanthan gum is produced by a specific type of bacteria when it ferments simple sugars from wheat, corn, soy, or dairy.
- Carrageenan is derived from seaweed.
- Lecithin is a natural extract from egg yolks, soybeans, and sunflower seeds.
Other food additive ingredients are synthetic compounds made in industrial labs rather than directly extracted from plants. These include:
- carbymethycellulose (also known as cellulose gum)
- polysorbate 80
- mono and diglycerides
Most of the eating patterns nutritional researchers are learning may help alleviate IBD symptoms recommend staying away from these types of food additives. While there’s no need to avoid these food additives unless they cause you symptoms, it may be worthwhile to explore and pay attention to whether these types of food additives cause or trigger symptoms for you.
Xanthan Gum
Xanthan gum is used as a thickener or stabilizer to improve a packaged food’s texture, consistency, flavor, and shelf life. It’s frequently added to gluten-free products because they can provide the elasticity and fluffiness that gluten gives traditional baked goods.
Common foods that contain xanthan gum are:
- gluten-free products
- salad dressings
- baked goods
- fruit juices
- soups
- ice creams
- sauces
- gravies
- syrup
- low-fat foods
While many foods contain it, note that most products have less than 1% xanthan gum added. Xanthan gum has been around for decades, and the FDA has approved this food additive and placed no limitations on the amount of xanthan gum a food can contain.
In human nutritional research studies, large doses of xanthan gum were found to have the following side effects [2]:
- increased frequency of bowel movements
- increased stool output
- softer stools
- increased gas
- altered gut bacteria
But these side effects don’t appear to occur unless a LOT is consumed…in a typical diet, it would be unlikely that you’d be eating as much as was consumed in that study. However, these are symptoms we care about, so it could be something for you to explore.
Carrageenan
Carrageenan is a type of seaweed that’s used to stabilize foods by making them gel. Although it’s been used for decades as a thickening agent in a wide variety of foods, there’s a growing body of evidence that’s raising questions about its safety, and several GI doctors I’ve talked to are growing concerned with carrageenan for IBD as well.
While most studies find that carrageenan is safe because it’s consumed in such small amounts, some studies have linked carrageenan to digestive diseases, inflammation, and even cancer [3]. More research is needed to have a definitive understanding of what carrageenan does to the gut and the body.
Carrageenan can be found in many foods, including:
- ice cream
- cheese
- chocolate milk
- plant-based milk alternatives
- breads
- jelly
- jams
- some processed lunch meats
- an alternative to animal-derived gelatin in some vegan foods
Maltodextrin
Maltodextrin is a white powder made from corn, rice, potato starch, or wheat. Even though it comes from plants, it’s highly processed. Maltodextrins are closely related to corn syrup solids, only differing in their sugar content.
Maltodextrin is generally used as a thickener or filler to increase the volume of a processed food. It’s also a preservative that increases the shelf life of packaged foods. It’s inexpensive and easy to produce, so it’s useful for thickening products such as:
- instant pudding
- gelatins
- sauces
- salad dressings
It can also be combined with artificial sweeteners like Splenda to sweeten products such as:
- canned fruits
- desserts
- powdered drinks
One reason to limit maltodextrin is to keep your gut bacteria healthy. According to a 2012 research study [4], maltodextrin can change your gut bacteria composition in a way that makes you more susceptible to disease. It can suppress the growth of probiotics in your digestive system, which are important for immune system function. The same study showed that maltodextrin can increase the growth of bacteria such as E. coli, which is associated with inflammatory bowel disease.
Sugar Alcohols
When checking an ingredient list, any ingredient that ends in “-ol” means that it’s a sugar alcohol (for example: sorbitOL, mannitOL, xylitOL).
One drawback with sugar alcohols in foods is that they’re absorbed more slowly in the small intestine than other sugars, which can lead to diarrhea, abdominal pain, and gas. For this reason, sugar alcohols are definitely not recommended during flares, but really, I don’t normally recommend them for people with IBD in general.
So where can you find sugar alcohols? Food products labeled sugar-free, including:
- hard candies
- cookies
- chewing gums
- soft drinks
Sorbitol is the most widely available sugar alcohol, manufactured from corn syrup. Sorbitol is frequently used to maintain the moistness in marshmallows and shredded coconut, as well as used in sugar-free candies.
Interestingly, a substantial amount of sorbitol is found naturally in dried plums (prunes), which causes the laxative effect this fruit is known for.
Artificial Sweeteners
People with IBD may want to limit artificial sweetener consumption. For example, a study published in 2018 examined the impact of Splenda, which is made up of 1% sucralose and 99% maltodextrin, on the gut microbiome and Crohn’s disease-like small intestine inflammation. This was an animal study, in mice, and results showed that while Splenda may alter the gut microbiome in both healthy and Crohn’s-prone hosts, the mice with Crohn’s showed increased inflammation [5].
While we need more research in humans, it can be something to keep in mind as you’re exploring what your trigger foods are.
Polysorbate 80 and Methycellulose
Polysorbate 80 is made from polyethoxylated sorbitan, which is a chemical compound derived from dehydration of a sugar alcohol. It’s used as a emulsifier or defoamer in foods – often used in ice creams or puddings to keep the creamy texture without separating and can also be used to bulk foods up and keep sauces smooth.
Methylcellulose is a chemical compound derived from treating vegetable cellulose with a chemical agent to create a tasteless, colorless powder. This powder is commonly used as a binding or thickening agent in many foods like ice creams, breads, cakes, and chocolate.
Methylcellulose also aids the absorption of water into the intestines, which helps make stools softer, so it’s a common ingredient in laxatives like Citrucel.
In mouse experiments, polysorbate 80 and methylcellulose can change the species composition of gut bacteria and induce or trigger intestinal inflammation, and even increase intestinal permeability [3,6,7]. We need human studies showing this too, but it can be something to keep in mind.
An example of how to put this into practice:
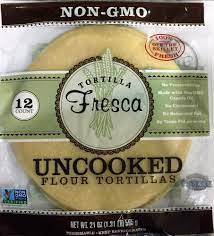
Let’s compare the ingredients in two tortillas (please note that I am NOT sponsored or paid to mention either of these products, I simply want to demonstrate that not all types of food products found on shelves are formulated in the same way):

The tortilla on the left is being marketed as plant-powered and having protein. But when you look at the ingredient list, there are a few ingredients inside that make me wonder…is this necessary? For example, see how it has modified wheat starch, pea protein, hydrogenated soy oil, caramel coloring, cellulose gum, and sucralose (which is Splenda)? Those are ingredients for IBD that I wouldn’t necessarily recommend.
Now compare that to the tortilla variety on the right, which has fewer, more minimal ingredients. This brand is refrigerated, and I’ve found that refrigerated tortillas tend to have fewer additives than their shelf-stable, highly preserved counterparts.
So really, the take home message here is to take the time to compare your options when it comes to the convenience foods upon which you rely heavily. It’s a small but proactive thing you can do toward shifting your diet to simpler, less processed foods, without making yourself unnecessarily crazy about occasional intake of food additives.
Ingredients are listed in order of quantity
One thing to mention for packaged goods with more than one ingredient, the ingredients will be listed in descending order by weight, so those with the largest amounts will be listed first. In other words, product ingredients are listed by quantity — from highest to lowest amount.
This means that the first ingredient is what the manufacturer used the most of.
So looking at the tortilla on the left, water is listed as the first ingredient on the list, meaning that these tortillas are mostly made up of water. And you’ll see that sorbic acid is listed last, meaning that this tortilla has the smallest amount of this chemical by weight, compared to the other ingredients.
How many ingredients should I look for in a packaged food?
While there’s no right answer here, try to stick with ingredients you can pronounce and with the fewest number possible. In general, I try to purchase packaged foods for my husband, who has Crohn’s disease, with 10 or fewer ingredients in it.
Take Home Message
Because these food additive ingredients are generally the mark of highly processed food, there is a case to be made for seeking out some simple swaps to reduce the number of these ingredients in your eating plan in favor of whole or more minimally processed alternatives.
Feeling confused on what to eat?
Has this led to a limited diet, weight loss, and/or fatigue?
I help my clients implement a highly personalized nutrition plan that brings clarity around which foods to add that may be beneficial, reduces fear and anxiety around eating, reduces inflammation, and ultimately helps them to get their lives back.
References:











































