IBD Constipation: Symptoms and Treatment for Ulcerative Colitis and Crohn’s
Danielle Gaffen, MS, RDN, LD
- Last Updated
Co-written by Renata Cauchon-Robles
Are you an IBD warrior experiencing constipation? IBD constipation can be relieved by some lifestyle changes and general management of IBD symptoms.
As an IBD dietitian, I’ve witnessed firsthand the distress constipation can cause for those with IBD, often complicating their condition. One particularly memorable experience was when my husband, Ari, who has Crohn’s disease, suffered such intense pain that we rushed to the ER, only to discover that constipation was the culprit. This incident not only reinforced the importance of managing constipation in IBD patients in my professional practice but also gave me a deeply personal insight into the challenges faced. Through a combination of dietary guidance, hydration, and lifestyle adjustments, I work with my clients to alleviate this often underrecognized IBD symptom, aiming to enhance their overall quality of life.
While IBD constipation is not the most reported symptom of Ulcerative Colitis or Crohn’s Disease, constipation can be something you experience. This article provides an overview of constipation; how to know if you’re experiencing it, and what to do about it.
What is Constipation?
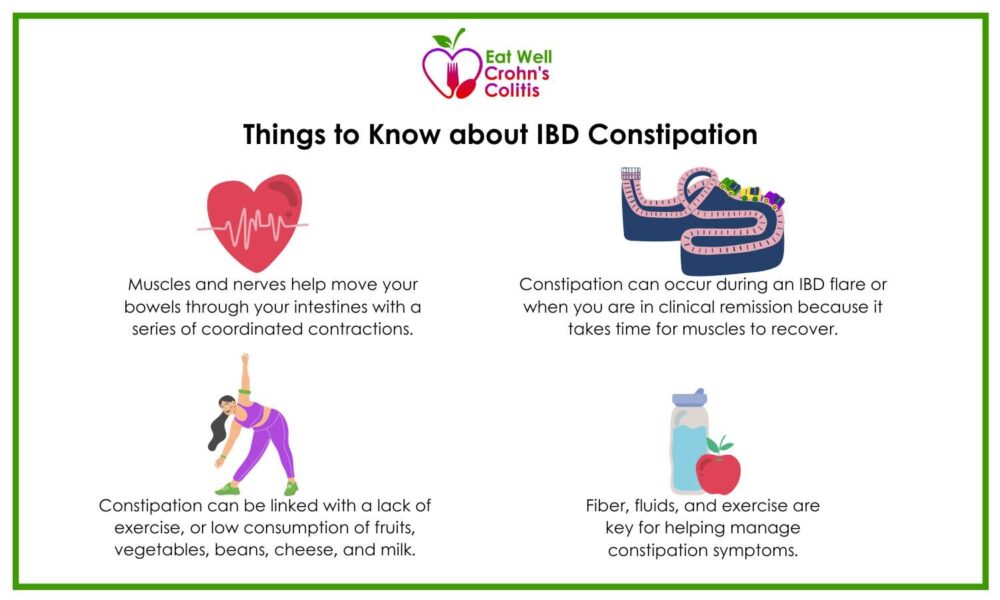
Your muscles and nerves are responsible for moving your bowels through your intestines with a series of contractions. It’s a synchronized dance that sometimes doesn’t flow perfectly. If the muscle cells aren’t functioning properly, are fatigued or uncoordinated, it can slow your intestines from emptying at a regular pace. This can also decrease how well your intestines absorb the nutrients from the food you eat.
Recognizing the signs of constipation is the next step in managing this uncomfortable IBD symptom. Here are some of the indicators that suggest you may be dealing with constipation.
How Do I Know If I’m Constipated?
Common symptoms that typically signal constipation include:
- straining during bowels
- hard or dry stools
- bloating
- excessive gas
- abdominal cramping
- feeling like you haven’t fully emptied after a bowel movement
Let’s explore how daily habits influence constipation relief.
Lifestyle’s Role in Constipation Relief
Lifestyle factors play a crucial role in the management of constipation. Studies have found a link between constipation and lack of exercise, as well as low consumption of fruits, vegetables, beans, cheese, and milk.
The discomfort caused by constipation goes beyond physical symptoms; it can also take a toll on your overall well-being.
Constipation and Quality of Life
Symptoms of constipation can decrease quality of life because they can be uncomfortable, cause pain, or may call for a change to eating habits. There is some association between chronic constipation (about 10 years) and the risk of developing colon cancer.
For those with Ulcerative Colitis, constipation can be a challenge. Understanding the nuances of constipation in the context of Ulcerative Colitis can help in better managing this symptom.
Navigating Constipation in Ulcerative Colitis: Understanding and Managing a Common Symptom
Ulcerative Colitis constipation can occur during a flare or when you are in remission. Overall, about 30-50% of people living with ulcerative colitis experience constipation more than 3 days a month. This is typically called proximal constipation where the location of the constipation may be close to an area of inflammation in your colon.
Since the inflammation and constipation can be close together, it can be hard to know what your symptoms are coming from. Paying attention to the texture and frequency of stools can give you helpful information. If you notice significant changes, talk to a healthcare professional about your symptoms.
The relationship between Ulcerative Colitis and constipation is complex, as the disease itself can influence bowel movement patterns. Let’s explore the science behind this phenomenon.
Can Ulcerative Colitis Cause Constipation?
Researchers have found that the muscles involved in bowel movements behave differently during an IBD flare than they do during remission. How quickly stool moves can also vary throughout the colon, such as moving faster in areas of inflammation or disease.
It can also take longer for muscles in diseased areas to recover, causing constipation symptoms to sometimes linger after clinical remission.
Considering the impact of Ulcerative Colitis on constipation, it’s worth examining how IBD in general may lead to this condition, whether through the disease’s symptoms or the treatments used.
Can IBD Cause Constipation?
Constipation can be a side effect of some medications prescribed for inflammatory bowel disease, such as vedolizumab (Entyvio). Other medications such as opioid pain medications can also cause constipation.
While constipation may not be the most common symptom of IBD, it may be more common in women living with IBD versus men living with IBD. In general, Crohn’s Disease constipation is less common than constipation associated with Ulcerative Colitis. Constipation is more common with irritable bowel syndrome (IBS) and hemorrhoids.
Inflammatory bowel disease constipation can still be experienced while you are in remission. This is because the muscles that help move your bowels don’t immediately recover.
While we know that IBD can lead to constipation, it is also crucial to understand the reverse—whether constipation can exacerbate or cause ulcers in individuals with IBD.
Can Constipation Cause Ulcers with IBD?
Ulcers are a characteristic of both Ulcerative Colitis and Crohn’s Disease. In Crohn’s Disease, the ulcers penetrate more layers of the intestinal lining. Straining during pooping can damage the lining of the colon, making it susceptible to sores or ulcers. However, ulcers can also be caused by other IBD disease activity that weaken the intestinal lining.
Examining the interplay between different gastrointestinal issues, we now turn to whether stomach ulcers, another common concern, can contribute to constipation.
Can Stomach Ulcers Cause Constipation?
There is minimal research on the connection between stomach ulcers and constipation. Constipation can be a symptom of rectal ulcers, and may be a longer term complication of untreated peptic ulcers.
Beyond understanding the causes, finding relief is paramount. Let’s discuss practical, at-home strategies for alleviating constipation, specifically for those with Crohn’s Disease.
How to Relieve Constipation with Crohn’s Disease
You may be wondering what you can do at home to alleviate your discomfort or concerns with constipation. Here are 3 ways to relieve inflammatory bowel disease constipation:
- Fiber: There are mixed studies on the role of fiber and constipation. Soluble fiber, combined with plenty of fluids can help get things moving. If there is an obstruction, however, fiber may not help.
- Fluids: Drink plenty of fluids. Set a goal of at least 8 cups per day. You may need even more with higher amounts of fiber. Fluid helps your body process fiber without discomfort.
- Exercise: Moving your body such as stretching, abdominal massage, or walking can support your body’s natural functions, including the muscles that help your intestines empty out.
Colitis Constipation Treatment
While home remedies can provide relief, some cases of colitis-related constipation may require more targeted treatments.
Depending on your symptoms and what stage of IBD you are experiencing, treatment may look different. Here’s what some of those treatments might involve:
- Laxatives or Stool Softeners. Macrogol or magnesium sulfate are sometimes prescribed for the short term to increase bowel activity.
- Mental Health. There is a connection between the gut and the brain. If a psychological condition is also present, supporting one can help relieve symptoms in the other.
- Biofeedback. Retraining the muscles around the intestines and pelvic floor has worked for people who haven’t responded to drug therapy. The pelvic muscles also play a part in supporting the movement of your bowels.
- Medical Scans. Some scans can provide useful information. A colonic manometry shows the activity of the intestinal muscles. Other scans like a CT scan or colonic scintigraphy use radiation and MRIs can be costly, so these aren’t very common. These are investigative techniques; they are not treatments.
As we’ve seen, addressing constipation in the context of IBD can be multifaceted. In summary, let’s recap the key takeaways to consider for managing this condition.
Take Home Message
IBD and constipation may feel like a lot to navigate, but paying attention to changes in your bowel activity can provide a lot of insight. Simple changes like adequate water intake, exercise, and fiber foods in your diet can help you get closer to feeling better.
Treatment plans may depend on what is causing your constipation. Connect with a doctor or dietitian to explore recommendations that will work best for your unique scenario.
For those eager to learn more and take further control of their IBD and constipation, the following resources can provide additional guidance.
Learn More
- Learn more about recommended fiber intake with IBD
- Build your own 7-day meal plan for Crohn’s and Colitis
- Learn about the difference between Ulcerative Colitis and Crohn’s Disease
References
- McQuilken SA. Gut motility and its control. Anaesthesia & Intensive Care Medicine. 2021;22(5):339-342. https://www.sciencedirect.com/science/article/pii/S1472029921000886. doi: 10.1016/j.mpaic.2021.04.002.
- Matsumoto T, Imai K, Goda Y, et al. Questionnaire Survey for Inflammatory Bowel Disease Patients in Japan; A Web-Based Japan, Crohn’s Disease, Ulcerative Colitis, Patients Survey. Crohns Colitis 360. 2023;5(4):otad069. Published 2023 Nov 17. doi:10.1093/crocol/otad069
- Arora G, Mannalithara A, Mithal A, Triadafilopoulos G, Singh G. Concurrent conditions in patients with chronic constipation: a population-based study. PLoS One. 2012;7(10):e42910. doi:10.1371/journal.pone.0042910
- Miller C, Emmanuel A, Zarate-Lopez N, Taylor S, Bloom S. Constipation in ulcerative colitis: pathophysiology and practical management. Frontline Gastroenterol. 2020;12(6):493-499. Published 2020 Aug 26. doi:10.1136/flgastro-2020-101566
- Bharucha AE, Wald A. Chronic Constipation. Mayo Clin Proc. 2019;94(11):2340-2357. doi:10.1016/j.mayocp.2019.01.031
- Massarrat, Sadegh; Saberi-Firoozi, Mehdi*; Soleimani, Asl†; Himmelmann, Günther W.‡; Hitzges, Michael; Keshavarz, Homa*. Peptic ulcer disease, irritable bowel syndrome and constipation in two populations in Iran. European Journal of Gastroenterology & Hepatology 7(5):p 427-433, May 1995.
- Christensen B, Colman RJ, Micic D, et al. Vedolizumab as Induction and Maintenance for Inflammatory Bowel Disease: 12-month Effectiveness and Safety. Inflamm Bowel Dis. 2018;24(4):849-860. doi:10.1093/ibd/izx067
- Angela J Khera, Janet W Chase, Michael Salzberg, Alexander J V Thompson, Michael A Kamm, Gut-Directed Pelvic Floor Behavioral Treatment for Fecal Incontinence and Constipation in Patients with Inflammatory Bowel Disease, Inflammatory Bowel Diseases, Volume 25, Issue 3, March 2019, Pages 620–626, https://doi-org.une.idm.oclc.org/10.1093/ibd/izy344
- Rectal Ulcer: Symptoms, Causes, Diagnosis, and Treatment. Healthline. Published January 8, 2024. Accessed April 14, 2024. https://www.healthline.com/health/rectal-ulcer#rectal-ulcer-symptoms
- Cleveland Clinic. Peptic ulcer disease. Cleveland Clinic. Published June 22, 2020. https://my.clevelandclinic.org/health/diseases/10350-peptic-ulcer-disease











































