Are Ulcerative Colitis and Crohn’s Disease Genetic?
Danielle Gaffen, MS, RDN, LD
- Last Updated
Co-written by Renata Cauchon-Robles
If you’re trying to understand more about how or why you developed inflammatory bowel disease (IBD), you might be wondering if ulcerative colitis (UC) or Crohn’s disease is genetic. Here is helpful insight to better understand your condition.
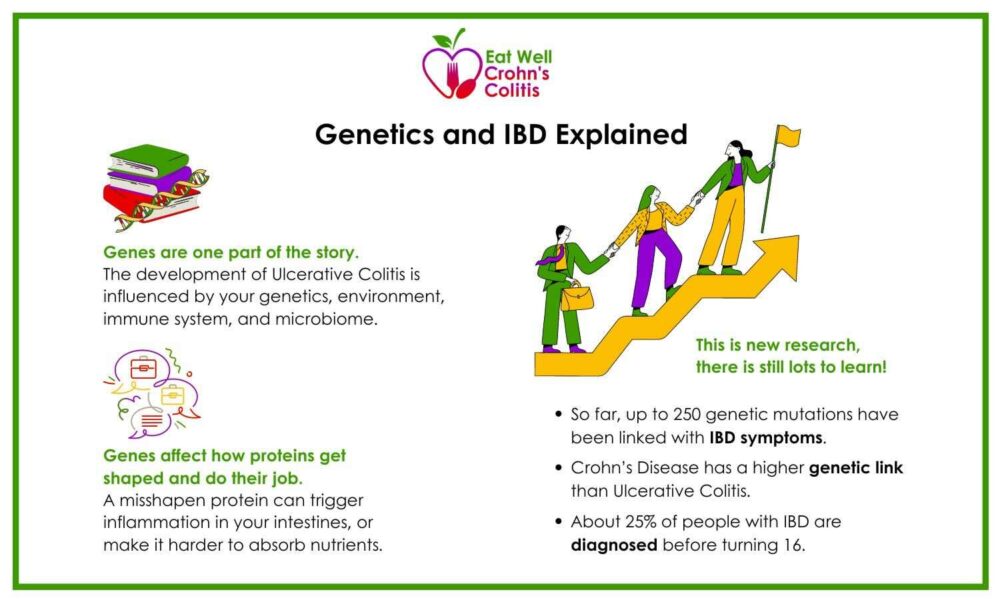
The exact cause of IBD is still unknown, but research shows that it is part of a complex interaction between our genes, our environment, our microbiome, and our immune system.
While you often hear Ulcerative Colitis and Crohn’s talked about together, they actually have unique characteristics. It is suspected that different genes play a role in how these diseases develop. Studies have shown that between 5% and 20% of people with IBD have a first-degree relative, such as a parent, child, or sibling, who lives with Crohn’s or Ulcerative Colitis.
Researchers are still learning more about the exact role of genes and IBD. They continue to test individual types of genes or gene mutations. With more research, we hope to learn just how our genes interact with our environment in a way that impacts the development of IBD. This article will provide helpful information about your genes and IBD.
Is Ulcerative Colitis Genetic or Environmental?
Ulcerative colitis is influenced by both genetic and environmental factors. Your immune system and your gut microbiome both play a big role in the development of ulcerative colitis. Specifically, your immune system plays a key role in inflammatory activity, including in the gut.
Your environment and your genes interact in many ways. It’s a complex dance and having imbalances in one can influence changes in the other.
Is Ulcerative Colitis or Crohn’s Disease Genetic?
It still isn’t exactly known whether UC and Crohn’s disease can be considered genetic diseases. Researchers are asking this very question!
So far, it has been found that up to 250 genetic mutations or disorders are linked with IBD symptoms. But we don’t know exactly what that means or how that might impact recommended treatments. It wasn’t until 2001 that a specific gene was identified as potentially increasing someone’s chances of developing Crohn’s disease.
Is Ulcerative Colitis or Crohn’s Disease Hereditary?
You may be wondering, is IBD inherited? Well, having a family member with IBD does increase the risk of developing the disease. Interestingly, the genetic risk seems to be greater with Crohn’s disease than Ulcerative Colitis.
Crohn’s can sometimes be confused with or have overlapping symptoms with Celiac disease. Celiac disease is an autoimmune condition that does have a higher rate of being hereditary.
Is Ulcerative Colitis or Crohn’s Disease Recessive or Dominant?
Let’s take an even closer look at these genetics. Several genes have been identified as important in the immune response and inflammation pathways in UC. Their role in UC is not about being dominant or recessive but about their involvement in key biological processes that contribute to the disease. More research is needed to fully understand the specific mechanisms by which these genes affect UC.
Researchers have found that inheriting a recessive gene mutation in the TNFSF15 gene may be linked with an increased risk for Crohn’s disease.
In early-onset Crohn’s disease, which is diagnosed in children under 5, a recessive gene known as NOD2 has been associated with the disease. Research completed in 2021 found that adults with mutations in this gene accounted for about 7-10% of people with IBD.
How Can Genes Affect IBD?
Since genes affect how proteins are created throughout the body, and proteins are responsible for all the different functions of our cells, some cells might behave differently when the original gene is different than expected. This could lead to inflammation or changes in absorption.
Researchers have found that genes show up differently in intestinal tissue when it is inflamed, especially in some of the genes that are responsible for transporting products (like nutrients) throughout the body.
Examples of Nutrigenomics Research for IBD
- Vitamin A and the BCM01 gene: A SNP in BCMO1 impairs beta carotene conversion to vitamin A, causing deficiencies that affect immune function and gut health, critical for IBD.
- Fructose and the TXNIP gene: TXNIP expression increases with fructose intake. However, in UC, a SNP decreases its expression, leading to bloating, pain, diarrhea, and fructose intolerance.
- Brassica Vegetables and the GSTM1 gene: Broccoli, cauliflower, cabbage, and Brussels sprouts increase inflammation in GSTM1-positive individuals but not in GSTM1-negative ones. Knowing GSTM1 status helps manage diet for IBD.
- Mushroom Intolerance and the OCTN1 gene: A SNP in OCTN1 is linked to mushroom intolerance in Crohn’s disease.
Understanding these genetic factors may help tailor nutrition advice to manage symptoms and ensure adequate nutrient intake in the future. Please visit our blog on nutrigenomics for more insights on this topic.
Are You Born with Ulcerative Colitis or Crohn’s Disease?
Having UC or Crohn’s disease since the first year of life is very rare. Some genetic disorders can lead to what’s called early-onset IBD where someone as young as 2 or 5 years old can develop the disease. And about 25% of people with IBD are diagnosed before turning 16.
In my practice, I’ve seen a wide range of ages at diagnosis. My husband, who has Crohn’s disease, was diagnosed at 17 years old. Many of my clients have been diagnosed around puberty, although I have also seen much younger and older diagnoses. This broad spectrum highlights that while early-onset IBD is rare, it is certainly possible, and individuals can develop these conditions at various stages of life.
Ulcerative Colitis or Crohn’s Genetic Testing
In general, Nutrigenomics or Precision testing will not tell us the whole picture.
For example, the popular genetic test such as 23 and Me will not show you the genes specifically involved in ulcerative colitis or Crohn’s disease. The specific gene most commonly associated with IBD is the gene NOD2. It is part of the immune system which helps fight bacteria in the intestinal tissue.
When clients ask about genetic testing, I explain a few caveats:
- More Research Needed: This field is still relatively new and unfortunately, there’s not a lot of funding in this area. We need more comprehensive studies to make this information clinically useful.
- Cost Factor: While it’s getting cheaper to have your entire genetic code sequenced, it’s still cost prohibitive for the average person. The gene sequencing you get from a company like 23andMe or Ancestry.com is only a cross-section of someone’s genome, not the entire DNA sequence. This cross-section doesn’t provide enough data for us to create a complete dietary prescription.
- Bigger Picture: Precision nutrition involves more than just nutrigenomics. Epigenetics and microbiomics are also crucial pieces of the puzzle.
In summary, more research is still needed to fully understand how genetics play a role in IBD.
Take Home Message
Genes have been found to play a role in the development of IBD. Research is still being done to see how big of a role they play and what that might mean for treatment options. For now, what is clear is that the microbiome and the environment are very important influencers in the development of IBD.
Learn More
- Learn more about nutrigenomics and IBD here
- Take a peek at how hair loss and IBD are connected
References
- Annese V. Genetics and epigenetics of IBD. Pharmacol Res. 2020;159:104892. doi:10.1016/j.phrs.2020.104892
- Loddo I, Romano C. Inflammatory Bowel Disease: Genetics, Epigenetics, and Pathogenesis. Front Immunol. 2015;6:551. Published 2015 Nov 2. doi:10.3389/fimmu.2015.00551
- Hu, S., Uniken Venema, W.T., Westra, HJ. et al. Inflammation status modulates the effect of host genetic variation on intestinal gene expression in inflammatory bowel disease. Nat Commun 12, 1122 (2021). https://doi.org/10.1038/s41467-021-21458-z
- What is Celiac Disease? | Celiac Disease Foundation. (n.d.). Retrieved from https://celiac.org/about-celiac-disease/what-is-celiac-disease/#:~:text=Celiac%20disease%20is%20hereditary%2C%20meaning,after%20people%20start%20consuming%20gluten
- Zhou Y, Zhu Y, Jiang H, et al. Polymorphism rs6478109 in the TNFSF15 gene contributes to the susceptibility to Crohn’s disease but not ulcerative colitis: a meta-analysis. J Int Med Res. 2020;48(10):300060520961675. doi:10.1177/0300060520961675
- Horowitz JE, Warner N, Staples J, et al. Mutation spectrum of NOD2 reveals recessive inheritance as a main driver of Early Onset Crohn’s Disease. Sci Rep. 2021;11(1):5595. Published 2021 Mar 10. doi:10.1038/s41598-021-84938-8
- Leung WC, Hessel S, Méplan C, et al. Two common single nucleotide polymorphisms in the gene encoding β-carotene 15,15′-monoxygenase alter β-carotene metabolism in female volunteers. FASEB J. 2009;23:1041-1053. doi:10.1096/fj.08-121962.
- Takahashi Y, Masuda H, Ishii Y, Nishida Y, Kobayashi M, Asai S. Decreased expression of thioredoxin interacting protein mRNA in inflamed colonic mucosa in patients with ulcerative colitis. Oncol Rep. 2007;18:531-535. doi:10.3892/or.18.3.531.
- Laing B, Han DY, Ferguson LR. Candidate Genes Involved in Beneficial or Adverse Responses to Commonly Eaten Brassica Vegetables in a New Zealand Crohn’s Disease Cohort. Nutrients. 2013; 5(12):5046-5064. https://doi.org/10.3390/nu5125046
- Petermann I, Triggs CM, Huebner C, et al. Mushroom intolerance: a novel diet-gene interaction in Crohn’s disease. Br J Nutr. 2009;102(4):506-508. doi:10.1017/S0007114509276446